People・Discovery
Sharing by Alumnus Dr Alex Wong Chun-wai
Knowledge on Immunotherapy for Cancer

Alumnus Dr Alex Wong is committed to conducting cancer immunotherapy research to benefit cancer patients.
Alumnus Dr Alex Wong Chun-wai (Biology) graduated from HKBU with first-class honours and received the Scholastic Award for his outstanding academic performance. Triggered by his grandfather’s death from cancer, he aspired to conduct research in cancer therapy. Consequently, he engaged in cancer immunotherapy research for his final-year project at HKBU under the supervision of Professor Ken Yung.
After graduation from HKBU, Alex continued to focus his research on cancer therapy and was awarded the Hong Kong Scholarship for Excellence Scheme (HKSES) in 2019, for which approximately 8% of applicants were selected in his award year. With the Scholarship awarded, Alex strived to deepen his understanding in cancer immunology at the University of Manchester (UoM) in England. He completed his PhD in Cancer Sciences in 2023 under the supervision of Dr Adam Hurlstone. His doctoral dissertation explored how to reverse resistance to immunotherapy for cancers such as colon cancer and skin cancer by targeting a protein called poly(ADP-Ribose) polymerase family member 14 (PARP14).
His findings were published in the prestigious cancer immunotherapy journal Nature Communications. This achievement marks the beginning of Alex’s lifelong commitment to conduct cancer immunotherapy research to benefit cancer patients.
Alex completes his PhD in Cancer Sciences in 2023 at the University of Manchester, England.
1. Please explain the mechanism of immunotherapy. Are all cancer patients suitable to receive immunotherapy?
Immunotherapy boosts our immune system to fight cancer. The immune system includes the lymph glands, spleen and white blood cells. Normally, it can spot and destroy faulty cells in the body, preventing cancer from further development. However, cancer might develop when the immune system recognises cancer cells but is not strong enough to kill them; or when cancer cells produce signals that stop the immune system from attacking them; or when cancer cells hide or escape from the immune system. There are different types of immunotherapies, including monoclonal antibodies, checkpoint inhibitors, vaccines, cytokines, and CAR-T cell therapy.
My doctoral study focused on the utilisation of checkpoint inhibitors. Checkpoint proteins are found on the surface of cells: PD-1 is found on the body’s T cells, and PD-L1 is found on normal cells. In general, PD-L1 binds with PD-1 to prevent T cells from being too strong which can destroy healthy cells in the body. However, cancer cells also present themselves as PD-L1 and therefore to ‘trick’ T cells by binding their PD-L1 with the T cells’ PD-1, avoiding recognition and preventing the T cells from killing them. Blocking the binding of PD-L1 to PD-1 with immune checkpoint inhibitors allows the T cells to recognise and kill cancer cells.
Each type of cancer is unique. Immunotherapy does not work for all types of cancer or for all people with cancer. However, doctors are continuing to try new treatments. Currently, immunotherapy has been proven to work in the following types of cancer: bladder, brain, breast, cervical, childhood, colorectal, esophageal, head and neck, kidney, leukemia, liver, lung, lymphoma and melanoma. In general, about 15 to 20% of cancer patients can overcome this disease by immunotherapy. However, there is still a majority of patients who do not yet benefit from it.
Alex (left) reunites with his HKSES fellow at the American Association for Cancer Research (AACR) Annual Meeting in the United States.
2. What is the difference between immunotherapy and other therapies in curing cancer?
Immunotherapy harnesses and enhances the natural powers of the immune system to work against disease by enabling the system to recognise, target and eliminate cancer cells throughout the body. It can be more targeted, selectively attacking cancer cells while minimising damage to healthy cells.
Other therapies like chemotherapy and radiation can destroy the DNA inside cells. This damage can stop them from growing. Our normal cells have a repair system to fix this damage, but cancer cells do not. As the damage builds up, these cancer cells keep trying to divide, and the damage eventually leads to their death. Generally, these treatments are less targeted and impact a wide range of rapidly dividing cells, which can lead to side effects.
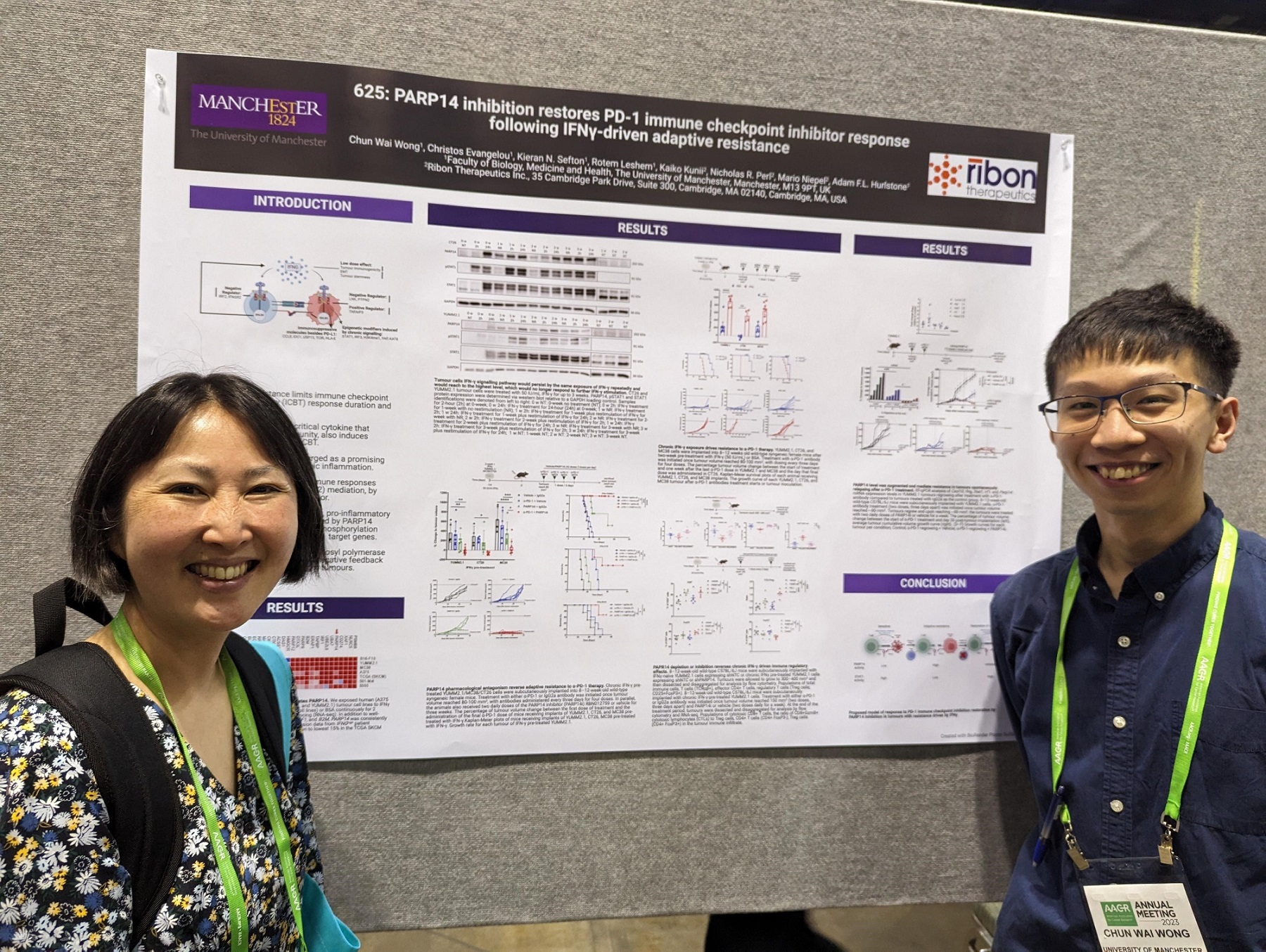
Alex (right) takes a photo with Dr Kaiko Kunii (left) from Ribon Therapeutics, one of his collaborators, after his presentation at the AACR Annual Meeting.
3. How can your research findings contribute to current cancer therapy especially immunotherapy? How can cancer patients be benefited if your research findings are translated to practical application?
Interferon-gamma (IFNγ) is an immune mediator characterised as a paradoxical protein with both pro- and anti-tumor functions. IFNγ can trigger processes in the body that directly kill cancer cells. However, IFNγ can also cause the body to produce molecules that slow down T-cells, which are the key components of the immune system to kill cancer cells.
Recently, as the first author, I published my findings in Nature Communications. The research revealed that exposure to chronic IFNγ conditions not only allows tumor cells to survive in the microenvironment but also induces a potent immunosuppressive microenvironment. Moreover, we identified a significantly upregulated enzyme, poly-ADP ribosyl polymerase 14 (PARP14), across human and mouse tumor cells treated with chronic IFNγ, inhibiting PARP14 reprograms tumor cells to exhibit a more immune-stimulatory phenotype, making them more likely to respond to PD-1 immunotherapy. In addition, PARP14 surprisingly can restrict T cells’ proinflammatory phenotype. Our work shows that stimulating T cells with a PARP14 inhibitor in long-term treatment results in T cells adopting a more proinflammatory phenotype, secreting more inflammatory cytokines which can kill cancer cells.
The discovery suggests that under tumor progression, tumor cells may undergo chronic IFNγ conditions, becoming resistant to immunotherapy. However, with PARP14 inhibitor intervention, the tumor microenvironment is completely reprogrammed, inducing T cells to produce more inflammatory cytokines, hence restricting tumor growth. This strategy can be combined with PD-1 immunotherapy to reinvigorate and strengthen anti-tumor immunity.
In this project, we teamed up with Ribon Therapeutics, Inc. (RTx), a biotech company that is working on creating new drugs to treat cancer and inflammation. Their approach involves targeting the emergency response systems inside cells that help them cope with stress. This collaboration uncovered that RTx’s PARP14 catalytic inhibitor (RBN012759) has a striking synergy with immunotherapy in the preclinical tumor models that we developed. The preclinical findings suggest that patients who progressed on immunotherapy might benefit from treatment with RTx’s PARP14 inhibitor.
Currently, at least 50% of cancer patients experience T cell exhaustion when treated with immunotherapy. This condition implies that T cells no longer secrete sufficient inflammatory cytokines, potentially leading to tumor recurrence and eventual mortality. This underscores the urgent need for a new target to rejuvenate T cell activity. My work demonstrates the significance of PARP14 in inhibiting T cell function in the anti-tumor response.
This work not only provides a key insight into how chronic IFN signaling in cancer cells drives immunotherapeutic resistance but also offers a new avenue for therapeutic targeting. Notably, drugs that inhibit PARP14 are currently in development. I believe my work would lay a solid foundation to test this new class of PARP14 inhibitors in clinical trials as an approach to reverse resistance and improve the overall efficacy of cancer immunotherapy.





